Now, more and more women are having babies in their mid to late 30s and early 40s. As a Maternal-Fetal Medicine specialist, I enjoy caring for my patients and seeing their families grow.
A question that can come up as people plan for a child or more children is, how old is too old to have a baby? Sometimes that’s answered by biology. Pregnancy after age 50 is extremely rare without the aid of assisted reproductive technology. But more often, unless there is a fertility issue, the answer is up to you and your comfort level. There are, however, some things to consider and steps you may want to take depending on your age.
What is considered advanced maternal age to have a baby?
Advanced maternal age by medical definition is anyone who is age 35 or older at the baby’s due date. Historically, this was when the risk of a having a baby with a chromosomal problem was about equal to the risk of the procedures to find out. Since then, newer laboratory techniques are available to help screen for these conditions with high accuracy and without risking the pregnancy.
What risks to baby and mom increase with a mother’s age?
While risks do increase with age, medical technology has improved over the years. We have more tests and techniques available to help moms and families determine the potential for a birth defect and prepare if that is a possibility. We also have enhanced treatment options for some situations such as heart problems.
To understand risks, preconception counseling is available and often recommended.
Down Syndrome and Other Chromosomal Risks
It’s important to understand that the risk of a chromosomal problem at age 40 is just 1 percent. Down syndrome (also known as Trisomy 21) is one of the more common chromosomal conditions that increase with a mother’s age. The National Down Syndrome Society quotes a risk of:
- 1 in 1,200 at age 25
- 1 in 350 at age 35
- 1 in 100 at age 40 (1 percent)
- 1 in 10 at age 49
Other chromosomal conditions that increase with a mother’s age are Trisomy 18 and 13.
Additional risks
- After age 35: Slight increased risk of congenital heart disease
- After age 40: Increased risk for: Gestational diabetes, gestational hypertension, having a small baby, cesarean section, miscarriage and twins
Effect of overall health on pregnancy
As women age, conditions such as diabetes, high blood pressure and lupus are also more common. These medical conditions may complicate pregnancy. However, with monitoring and care a healthy pregnancy for mom and baby can be achieved.
It is important to note that even with these increased risks, with appropriate care and close monitoring the vast majority of women over age 40 will have healthy and happy pregnancies.
What tests/screenings should be considered for pregnant women over age 35?
Chromosomal Screenings
The accuracy of these screenings has improved significantly over the years. In the past, the screening tests were not very accurate. While the detection rate was 80-95 percent, the false positive rate was 2.5-25 percent, meaning 2.5-25 percent of the people that took the test were told their baby may have Down syndrome or were mistakenly told their baby did have Down syndrome. Ultrasound can be used to screen for Down syndrome but is only 75 percent accurate and has a 20 percent false-positive rate.
Newer screening tests called Cell Free DNA look at the fetal DNA in the mom’s blood. This simple blood test can be done as early as nine weeks (although I prefer to do this test at 11 weeks to decrease the chance of having to redraw the test because enough DNA was not present yet). The test is 99.7 percent accurate with a false positive rate <0.5 percent. It also looks for Trisomy 18 and 13, as well as the sex of the baby (great for those gender reveal parties!).
There are other abnormalities that can be screened for as well if you want, after discussing with your provider. In rare instances, test results are inconclusive. If this happens, it really just means we should monitor these patients more closely. Your provider can usually order this test.
Diagnostic testing, which involves putting a needle in the amniotic cavity (Amniocentesis) or placenta (Chorionic Villus Sampling – CVS) has a small risk of miscarriage. This test can be done to confirm abnormal findings of the Cell Free DNA screening. A Maternal-Fetal Medicine specialist usually does this test.
Congenital Heart Disease Screening
Women over 35 can be offered a specialized ultrasound called a Detailed Anatomical Survey and/or Fetal Echocardiogram. This test is done to determine the possibility of the baby having congenital heart disease or other birth defect. In our office, if the Detailed Anatomical Survey is normal, we do not do the Fetal Echocardiogram because it is unlikely to provide added benefit.
Why test for chromosomal abnormalities and other risks?
Some people may wonder why test for any of the risks, especially chromosomal abnormalities if you can’t change the outcome? The decision to test/screen is personal, and one that each woman/family must make for herself/themselves.
Here are some reasons people decide to do testing/screening.
1. To Know.
Most people just want to know “yes” or “no”. Fear of the unknown is far worse. With Zoe, I was surprised Tracy was anxious about getting the results back. When she had the test done 11 years ago, I didn’t recommend it because at that time it had a 25 percent false positive rate. However, having seen many 40-year-old patients in my practice I knew our odds were only 1 percent. Tracy would’ve loved Zoe with or without Down syndrome – she just wanted to know yes or no.
2. To Prepare.
A nurse I work with has a granddaughter with Down syndrome. She tells me all the time about her son-in-law. When he found out about the diagnosis before his child’s birth, he studied and researched it and what he learned was so helpful to know in advance. We have a great Down Syndrome Association for Families of Nebraska right here in Lincoln that he has been able to network with also.
3. To Take Action.
For some conditions, there are treatment options. Knowing the risk in advance will help determine the best course of action for mom and baby.
3 key factors for a healthier pregnancy at any age
Having a baby is a very natural and safe thing to do. We talk about increased risk with age because we want to identify and do our best to mitigate the risks for the best outcomes possible.
Three key factors all work together to achieve a healthier pregnancy for mom and baby at any age, and especially after age 35. Preconception counseling/early prenatal care, expertise of doctors and specialists, and women taking an active role in their care.
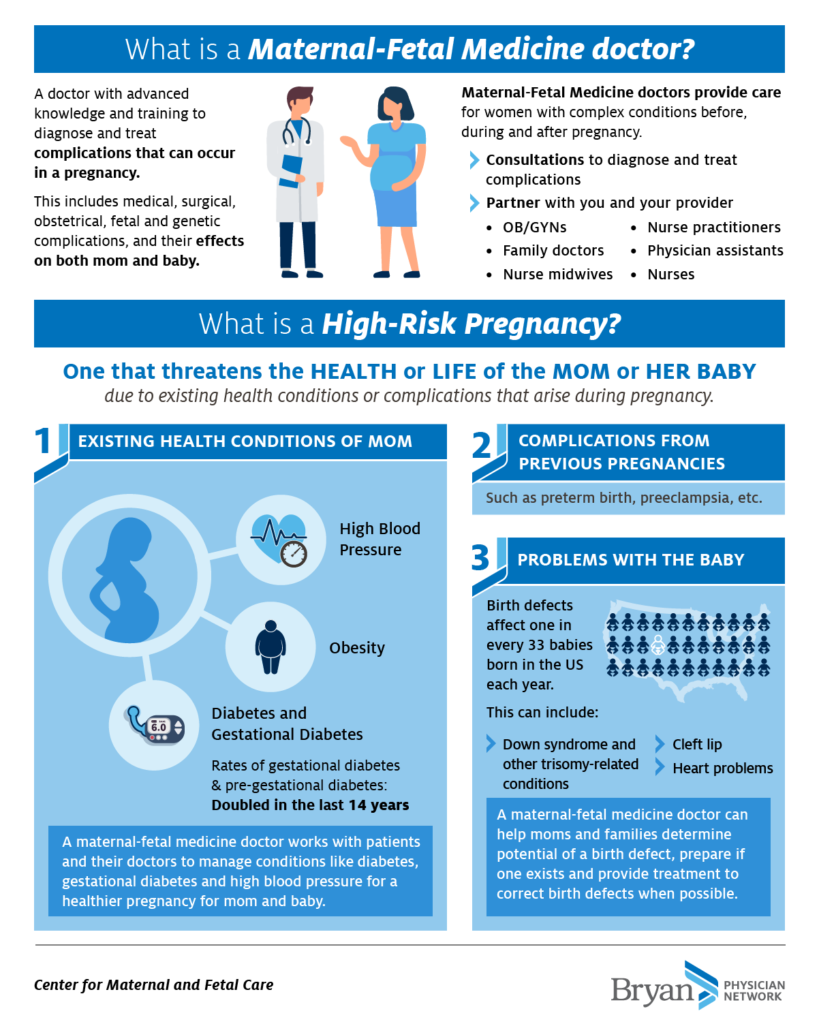
Get all this information and more in this infographic from Bryan Health’s Center for Maternal & Fetal Care!

Sean Kenney, MD
Maternal-Fetal Medicine Specialist
Dr. Kenney is a Maternal-Fetal Medicine specialist with the Center for Maternal & Fetal Care, part of the Bryan Physician Network.
He and his wife Tracy have nine kids and have lived in Lincoln for the last 20 years after he completed his fellowship.









